

Everlyne Khasoa holds her three-month-old son
close, his tiny fingers curled around hers.
She has done everything right, attended prenatal
checkups, taken her medication religiously, and followed every instruction
doctors gave her.
Yet for months now she battles a relentless
anxiety—the fear of running out of antiretroviral drugs that are her son’s
lifeline. For the past few months, the dispensary where she collects
life-saving antiretroviral (ARV) drugs for her baby has faced severe shortages.
She recalls the last time she left the clinic
with barely enough to cover their monthly dose.
“I felt helpless,” she says, her voice breaking.
“What kind of mother cannot protect her child?”
Everlyne was diagnosed with HIV five years ago.
She was assured that with strict adherence to
treatment, her child could be born HIV-negative.
For
nearly two years, her viral load has remained suppressed.
But the recurring stockouts of essential drugs,
especially zidovudine syrup, crucial in preventing mother-to-child
transmission, have left her in a terrifying predicament.
“I have had to ration my baby’s medicine,
knowing the risk,” she says. “It’s terrifying.”
And she is not alone. Across Kenya, thousands of
mothers living with HIV face the same uncertainty. What happens when
life-saving drugs are simply unavailable?
Deadly impact of stockouts
At a government clinic in Kakamega, Samuel
Mujera, a clinical officer specialising in HIV treatment, explains the grim
situation.
He has seen firsthand how stockouts erode years
of progress.
“Yes, we’ve had multiple shortages this year,”
he confirms. “Zidovudine syrup has been unavailable for almost a year, and
septrin syrup, which protects against opportunistic infections, has been
missing for three months.”
Mujera also mentioned a shortage of atazanavir
tablets, which are important for adults on second-line HIV treatment.
Atazanavir is effective when the first-line
treatment fails because the virus does not easily develop resistance to it.
“Between July and August last year, atazanavir
stock ran out,” he explained. “We had to ration the limited supplies available
while waiting for replenishments.”
Without these medications, the risk of HIV
transmission through breastfeeding increases significantly.
“We are left hoping that a single drug will be
enough,” Mr. Mujera admits. “But when a baby tests HIV-positive simply because
we lacked all the necessary drugs, it’s devastating.”
Many mothers, like Everlyne, are forced to travel long distances in search of alternative health facilities. Others, especially those in remote areas, have no choice but to wait and hope.
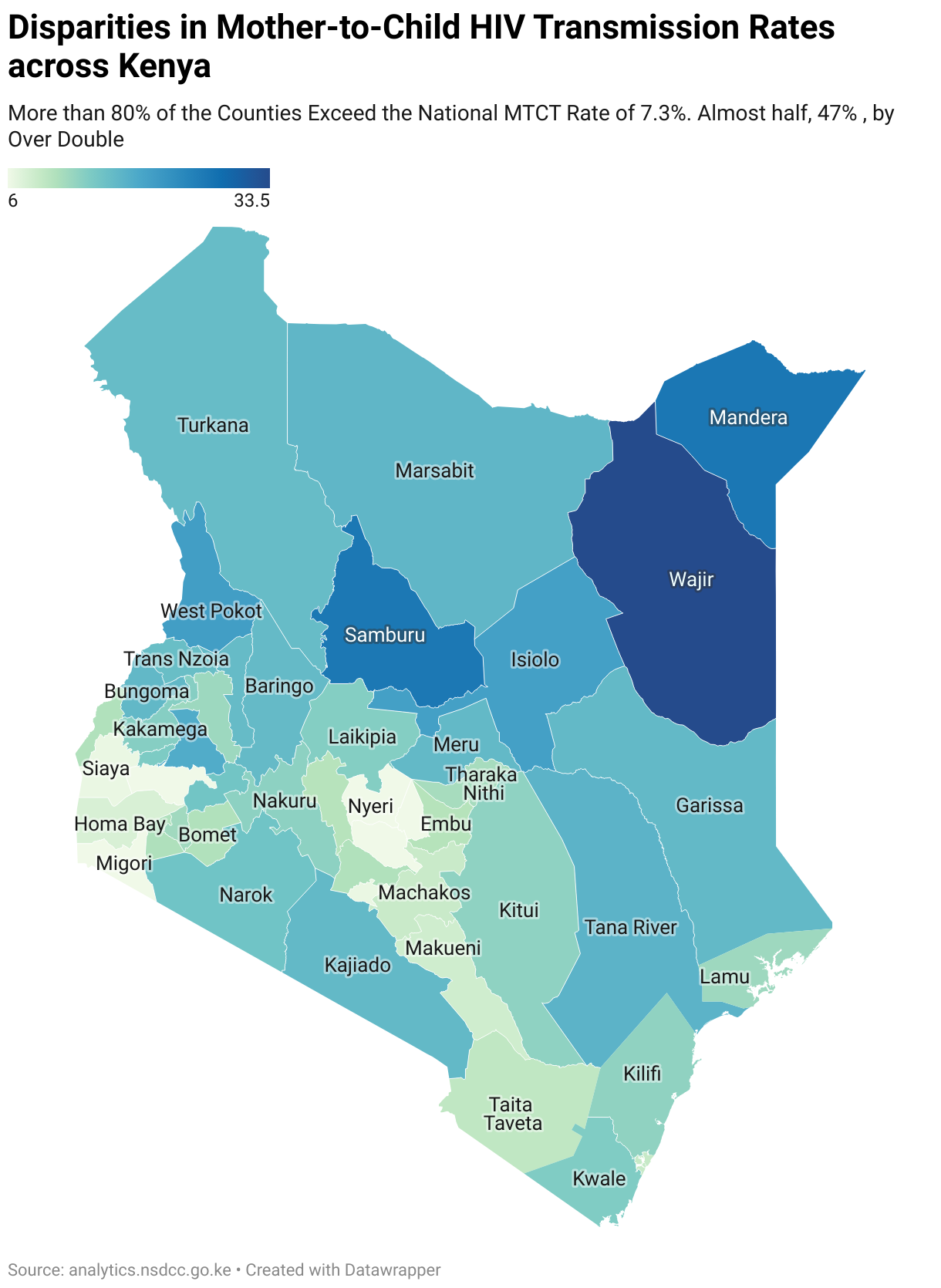
Kenya’s target is to reduce mother-to-child HIV
transmission below 5%, yet some counties, like Kakamega, still report rates as
high as 10-14%. The situation is dire.
Why these drugs matter
Dr. Joseph Maina, a research scientist at the
Kenya Medical Research Institute (KEMRI), explains why these particular
medications are so critical.
“There are three critical stages when
transmission is most likely to occur: during pregnancy, delivery, and
breastfeeding.
“In the uterus, the likelihood of transmission
is relatively low, between 15-30% without intervention,” he said. “However,
complications like severe trauma or infections can allow the virus to cross the
placenta.”
During delivery, the risk increases due to the
potential mixing of maternal and neonatal blood.
Breastfeeding presents another risk, as HIV can
be transmitted through breast milk, especially in the early months when an
infant's immune system is immature.
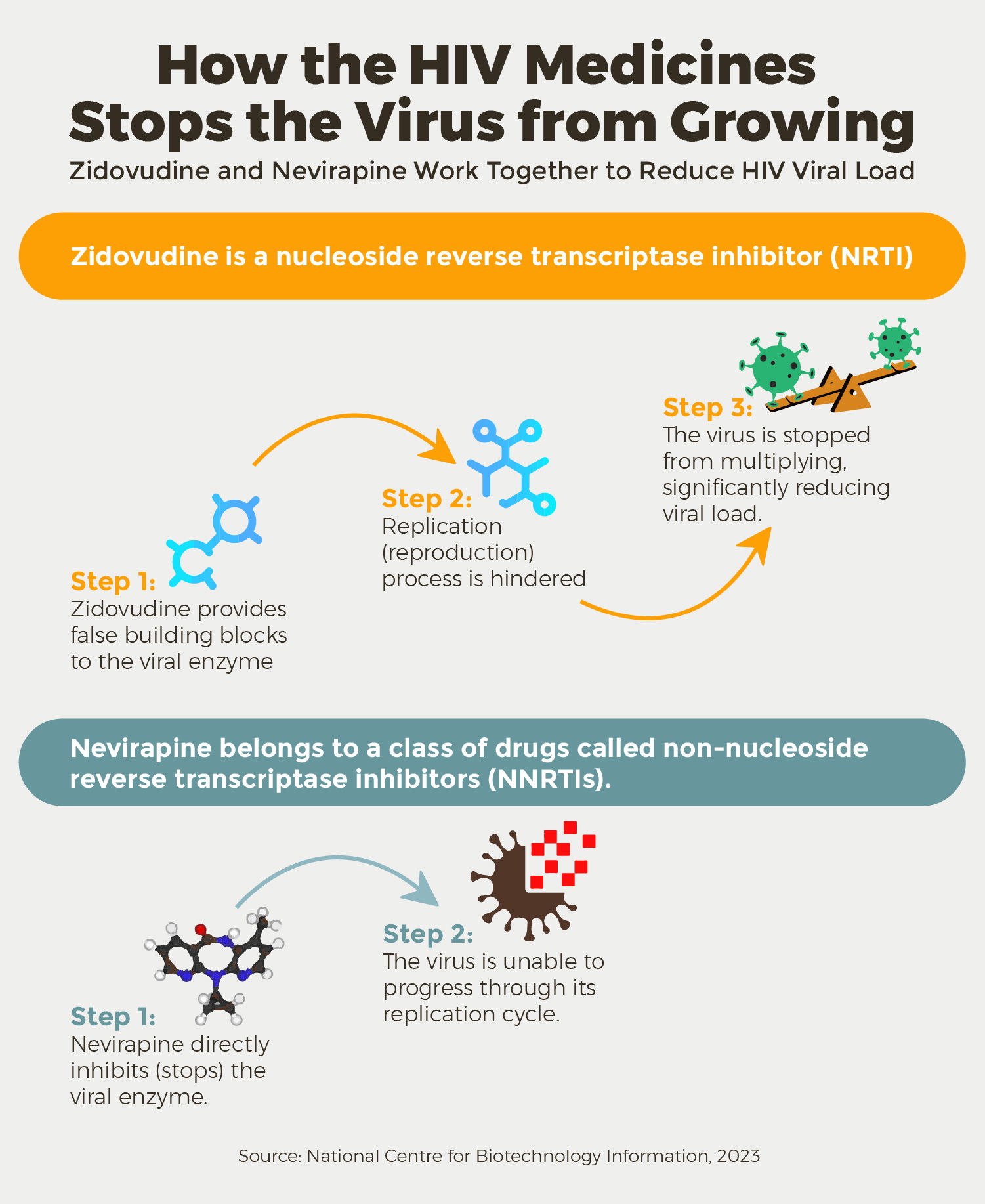
“These drugs work at different stages of
the virus’s life cycle. Zidovudine weakens the virus early, while nevirapine
blocks its replication. Used together, they provide the best chance of
preventing transmission.
“These two drugs are administered during pregnancy,
delivery, and breastfeeding to ensure maximum protection for both the mother
and the baby,” he said.
“The mother receives zidovudine and nevirapine
as part of a combination therapy to reduce viral load, while the baby is also
given prophylactic doses to provide additional protection after birth,” Dr.
Maina added.
The combination is also crucial because of
the issue of drug resistance. Drug resistance occurs in two ways: through
improper use of drugs; if drugs are not taken as prescribed, at the right
dosage and frequency, it can lead to the development of resistant strains of
the virus. Moreover, individuals may already have drug-resistant strains in
their system, which can then be transmitted to others, including from mother to
child. Combination therapy is very critical, as it makes it harder for the
virus to develop resistance to all the drugs being used simultaneously.
Reasons for stockouts
Stockouts of antiretrovirals (ARVs) in Kenya are
not new. Procurement delays, funding gaps, and reliance on donor supply chains
have made the supply of HIV medication unpredictable.
Dr. Evans Mbuki, Head of Health Products and
Technologies at the National AIDS & STI Control Programme (NASCOP),
explains that sometimes stockouts happen because only one manufacturer bids
during procurement.
“If that manufacturer experiences delays, we
face shortages. Earlier in 2024, we ran out of ARV suspensions for newborns due
to a production issue.”
To mitigate the impact of stockouts, he
recommends redistribution of stock within counties as a crucial strategy to
address localised shortages.
“Counties should establish stock levels
and consumption patterns across facilities to ensure equitable
distribution," said Dr. Mbuki.
Kenya’s HIV treatment programme depends heavily
on donor funding, with the latest data showing 63.5% of funding coming from external
sources.
“For us to stop relying on donors, the
government must invest more in HIV services. Counties need to allocate budgets
for healthcare workers, clinics, and supply chain management. Without this
commitment, service delivery will be compromised when donor funds diminish, and
for long-term sustainability, we must invest in local drug manufacturing,” Dr.
Mbuki warned.
Dr. Mbuki also highlighted the importance of
integrating HIV services into general healthcare.
“HIV is a chronic ailment like any other. We
need to move away from standalone Comprehensive Care Clinics (CCCs). Clinicians
should manage HIV patients alongside other cases like diabetes or antenatal
care. This integration would optimise workforce use and improve service
quality.”
Crisis looms
As of early this year, Kenya’s HIV treatment
landscape faces another major threat: funding uncertainty.
Historically, the United States’ President's
Emergency Plan for AIDS Relief (PEPFAR) has been a cornerstone of Kenya’s HIV
programmes.
Over the last two
decades, PEPFAR contributed approximately $8 billion. However, changes in international aid policies
have made this funding less secure.
A recent executive order from U.S. President
Donald Trump initiated a reassessment of U.S. foreign aid, leading to a 90-day
freeze on funding, including PEPFAR support.
This sudden halt has thrown Kenya’s HIV
treatment plans into jeopardy.
The Ministry of Health, alongside the Council of
Governors and key health agencies, has projected that Kenya needs at least Sh28
billion annually to sustain its HIV programmes.
Currently, donor support covers only a fraction
of this, leaving a $78 million funding gap, a shortfall that could translate
into even more drug shortages.
“Despite our best efforts, domestic funding for
HIV remains below target,” says a Ministry of Health official. “Only 34% of the
required funding has been raised domestically, far below the 50% goal set under
the Kenya AIDS Strategic Framework.”
Cost of a broken system
For clinical officers like Mr. Mujera, the
hardest part of the job is breaking the news to a mother that her child has
tested HIV-positive.
“You feel like you’ve failed her,” he admits.
“At six weeks, when we do the DNA PCR test, we pray for a negative result. If
the baby is positive, it’s heartbreaking.”
And yet, there are victories.
“When an HIV-exposed infant tests negative at
two years old, we celebrate. We dress them in gowns and cut cakes; it’s a small
victory in a long battle.”
But how many more children will miss out on
these celebrations if funding and supply chain issues persist?
Way forward
Kenya is now scrambling for solutions. President William Ruto,
speaking at PEPFAR’s 20th anniversary in Kenya, acknowledged the programme’s impact:
“In 20 years, PEPFAR has channelled over $6.5
billion into Kenya’s HIV response. As a result, we have seen an 83% reduction in new
infections and a 65% drop in HIV-related mortality.”
Yet, the question remains how can Kenya sustain
these gains without guaranteed foreign aid?
Several countries have successfully transitioned
to alternative funding models:
- South
Africa has significantly
reduced donor dependency by at least 70% by allocating more of its
national budget to HIV treatment.
Kenya could follow suit by prioritising HIV care in its domestic budget.
- Rwanda has integrated HIV treatment into its national health
insurance scheme, making care accessible to all citizens. Kenya’s Social
Health Insurance Fund (SHIF) could be expanded to cover ARVs
comprehensively.
- Uganda
has
leveraged private sector partnerships, with companies funding HIV
programmes. Kenya’s corporate sector, including telecom giants
like Safaricom, could play a bigger
role in bridging the funding gap.
The Kenyan government
has already pledged $10 million for the Global Fund’s Seventh Replenishment, a 67% increase from its previous commitment.
But this is only a start.
Fight is not over
Despite the looming crisis, health workers like
Mr. Mujera remain determined.
“We cannot end HIV transmission while babies are
still being born positive,” he says. “Science exists. The drugs exist. Now we
just need a system that works.”
For mothers like Everlyne, that future cannot come soon enough.
This article was produced as part of the
Aftershocks Data Fellowship (22-23) with support from the Africa Women’s
Journalism Project (AWJP) in partnership with The ONE Campaign and the
International Center for Journalists (ICFJ).










