
Investing in quality healthcare is not only a fundamental right but also a key driver of Kenya’s economic growth and social transformation, Health Cabinet Secretary Aden Duale said.
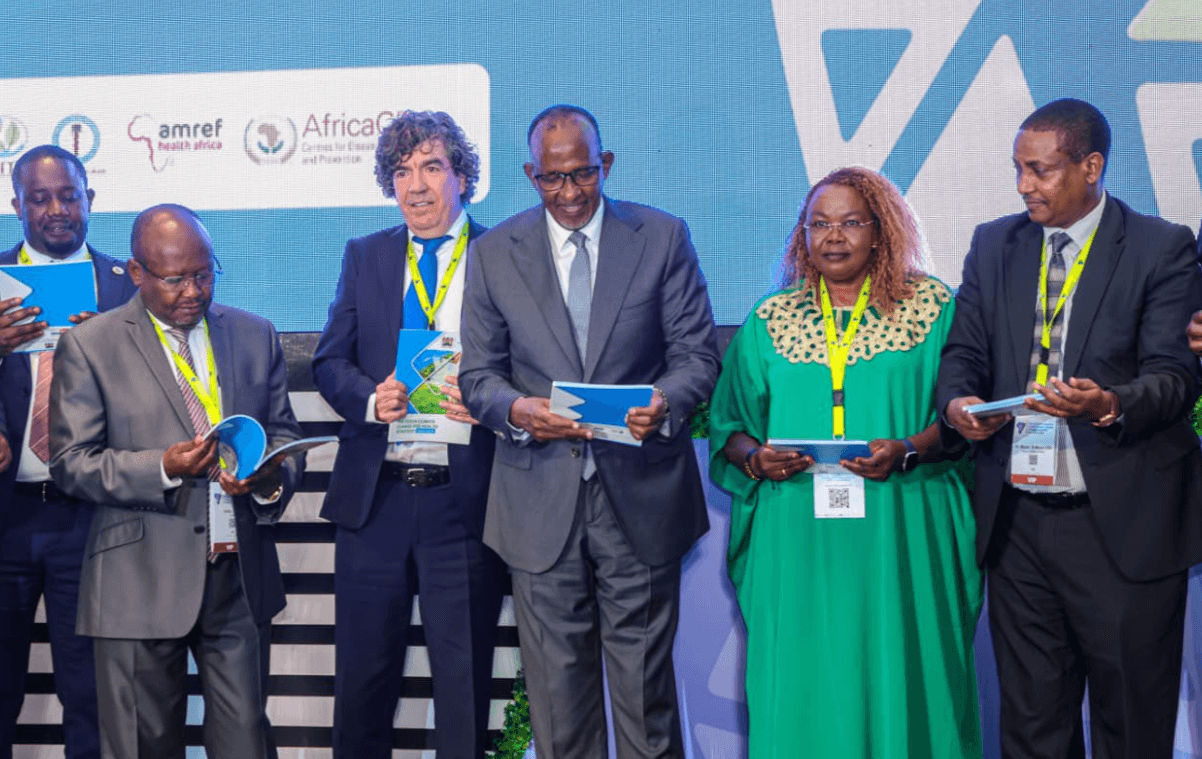
Speaking during the launch of three landmark reports in Nairobi — the Kenya Quality of Care and Human Resources for Health Assessment, the Service Availability and Readiness Assessment (SARA), and the Reproductive, Maternal, Newborn, Child and Adolescent Health and Nutrition (RMNCAH+N) Investment Case — Duale underscored the critical link between health and national development.
The reports, jointly developed by the Ministry of Health, county governments, private sector stakeholders, and development partners, provide an in-depth analysis of Kenya’s healthcare system.
The reports are said to highlight the strategic investments required to strengthen service delivery and fast-track progress toward Universal Health Coverage (UHC).
According to the findings, every shilling invested in quality healthcare yields a long-term return of approximately Sh12 in economic productivity, underscoring health as both a social and economic priority.
The CS said quality healthcare sits at the heart of the Bottom-Up Economic Transformation Agenda (BETA), which envisions inclusive, people-centered development.
He said a nation’s economic performance is directly linked to the well-being of its citizens, as good health enhances productivity, reduces poverty, and fosters growth.
“Investing in quality healthcare is not just a moral obligation; it is an economic imperative,” Duale said.
“Healthy citizens are more productive and better equipped to contribute meaningfully to national development.”
SARA covered 3,605 health facilities across all 47 counties and showed that while outpatient, maternal, and child health services are widely accessible, significant gaps persist in managing non-communicable diseases, mental health, cancer, and palliative care, particularly in rural and lower-level facilities.
Findings showed only 37 per cent of the 6,132 facilities offering delivery services had all seven signal functions for Basic Emergency Obstetric and Newborn Care (BEmONC).
Similarly, 46 per cent of Level 4 and 5 hospitals providing maternity services met all nine Comprehensive Emergency Obstetric and Newborn Care (CEmONC) standards.
All Level 5 facilities were fully compliant, compared to 44 per cent of Level 4 hospitals.
The report also identified a mismatch in service delivery, with some Level 2 and 3 facilities performing inpatient, surgical, and caesarean section procedures beyond their approved capacity — most of which were privately owned.
Duale said such inconsistencies compromise standardization and quality assurance in healthcare delivery.
Human resources emerged as another critical challenge.
The national core health workforce density — encompassing medical officers, clinical officers, nurses, and laboratory personnel — stands at 14.3 per 10,000 population, below the World Health Organization’s recommended 23 per 10,000 needed to achieve a 70 per cent UHC service index.
Only Nairobi, Kisumu, Mombasa, and Nyeri counties met this target.
While absenteeism among health workers has declined from 52.8 per cent in 2018 to 30 per cent in 2025, unplanned absences still disrupt service delivery.
Duale emphasized that the findings from the reports will guide ongoing policy and legislative reforms, including the Quality of Healthcare and Patient Safety Bill, currently before the Senate.
The Ministry intends to use the recommendations to strengthen facility readiness, reclassify facilities under the Kenya Essential Package for Health (KEPH), and implement a national human resource strategy to ensure fair deployment and retention of healthcare workers.
Other recommendations include institutionalizing continuous professional development, mentorship, enhanced clinical supervision, and ensuring universal access to treatment guidelines to standardize care across all health levels.
Duale expressed gratitude to development partners — including the Bill & Melinda Gates Foundation, the Global Fund, UNFPA, UNICEF, and the World Health Organization (WHO) — for their technical and financial support in developing the reports.
“These reports reaffirm our shared commitment to build a healthcare system that delivers quality, equity, and resilience for all Kenyans,” Duale said.
As Kenya advances toward Universal Health Coverage, the Ministry reaffirmed that prioritizing quality healthcare is both a social and economic investment.
A
healthy population, it noted, ensures a productive workforce, reduces
health-related poverty, and lays a strong foundation for sustainable economic
growth.













